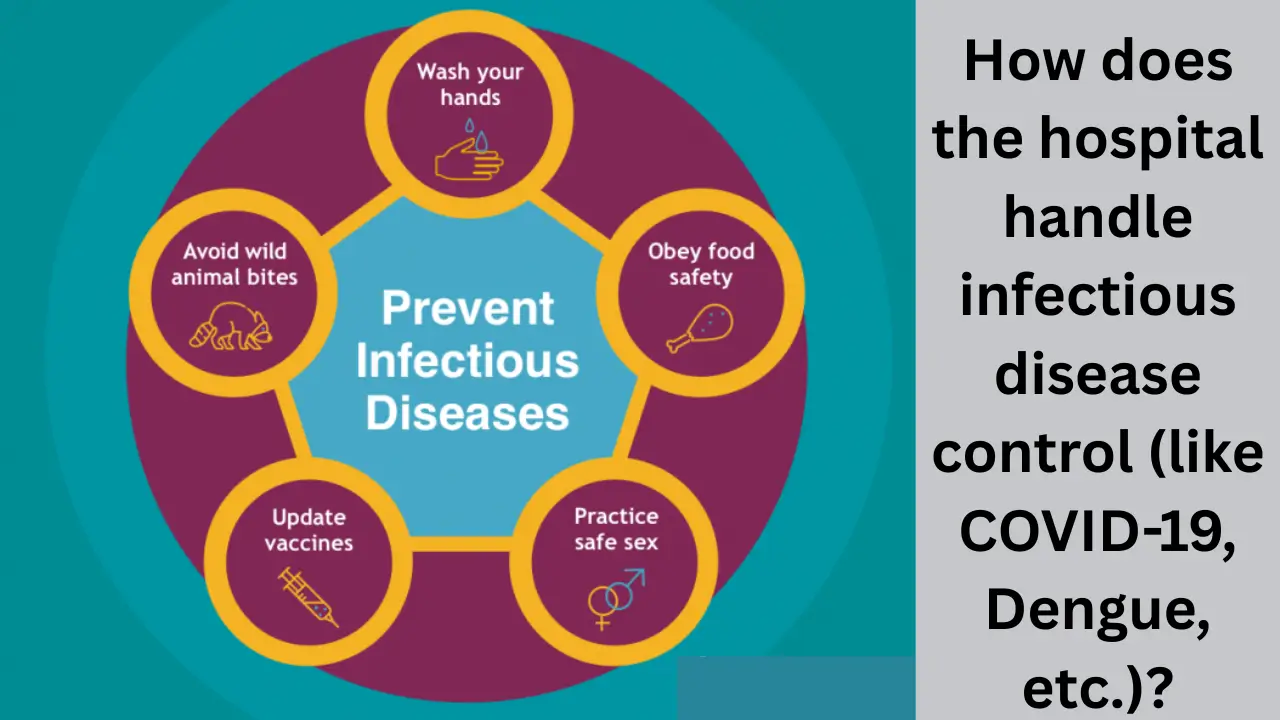
Infectious disease control in hospitals is a critical component of healthcare, especially during outbreaks of highly contagious diseases like COVID-19 and vector-borne diseases such as dengue. Hospitals implement comprehensive strategies to prevent the spread of infections within their facilities, safeguarding both patients and healthcare workers. The control measures encompass diagnosis, clinical management, environmental controls, staff training, and surveillance systems.
Infection Prevention and Control (IPC) Policies
Hospitals develop specific Infection Prevention and Control (IPC) programs tailored to infectious diseases. These programs include:
- Strict hand hygiene protocols: Regular hand washing and sanitizing reduce transmission risk.
- Use of personal protective equipment (PPE): Masks, gloves, gowns, and face shields are mandated when handling infectious patients.
- Isolation and cohorting: Patients with confirmed or suspected infections like COVID-19 or dengue are isolated to limit cross-infection.
- Environmental cleaning: Frequent disinfection of surfaces, medical equipment, and patient areas.
- Waste management: Safe disposal of infectious waste to prevent environmental contamination.
An IPC team, including infection control officers and nurses, oversees the daily implementation of these measures and provides ongoing training to healthcare workers.
Diagnosis and Surveillance
Hospitals employ multiple diagnostic methods for infectious diseases:
- Molecular tests (PCR): Used for COVID-19 diagnosis via respiratory samples, and dengue using blood or serum samples.
- Serological tests: Help detect antibodies specific to each virus to confirm past or current infection.
- Differential diagnosis protocols: Especially essential during overlapping outbreaks (e.g., COVID-19 and dengue) to correctly identify the causative agent.
- Surveillance systems: Monitor and report cases, helping to identify trends and outbreaks quickly.
Laboratories coordinate sample handling with strict biosafety protocols to minimize contamination and ensure safe transport and testing.
Clinical Management of Infectious Diseases
Hospitals adopt clinical care protocols focusing on:
- Early recognition and treatment: Timely diagnosis of diseases like dengue can prevent progression to severe forms.
- Supportive care: Such as oxygen therapy for COVID-19 patients and fluid management for dengue patients.
- Monitoring warning signs: Detecting symptoms like respiratory distress in COVID-19 or bleeding in dengue to escalate care promptly.
- Specialized care units: Dedicated isolation wards with appropriate air handling systems to treat infectious patients safely.
By managing mild cases in primary care and reserving hospital capacity for severe cases, hospitals avoid overwhelming resources.
Hospital Infrastructure and Air Quality Control
Dedicated wards for infectious disease management require specific infrastructure considerations:
- Negative pressure rooms: These prevent airborne pathogens from escaping the isolation area.
- Ventilation: Ensuring at least 12 air exchanges per hour using exhaust fans and limiting recirculation of air.
- Separate clean and contaminated pathways: To avoid cross-contamination of staff and patient traffic.
- Shower and changing areas: For healthcare workers to safely don and doff PPE.
During the COVID-19 pandemic, many hospitals upgraded HVAC systems and created temporary infectious disease units to adapt to the surge.
Staff Training and Workforce Management
Proper handling of infectious patients demands well-trained healthcare workers (HCWs):
- Intensive training: On PPE use, infection control protocols, and patient management in infectious disease units.
- Duty scheduling: Shifts are often limited (e.g., 6-hour shifts) to reduce fatigue from prolonged PPE use.
- Accommodation and quarantine: On-site facilities allow staff to isolate when required.
- Telemonitoring and CCTV: Real-time observation ensures compliance with safety protocols.
Reallocation of non-essential staff to infectious disease care areas is also common during outbreaks.
Managing Co-Infections and Multi-Disease Scenarios
In regions where diseases like COVID-19 and dengue co-circulate, hospitals:
- Develop integrated clinical protocols for the differential diagnosis and management of febrile illnesses.
- Screen for co-infections to optimize treatment and isolation strategies.
- Strengthen community engagement and vector control to reduce dengue spread while controlling COVID-19 transmission.
Table: Key Measures in Hospital Infectious Disease Control
| Aspect | COVID-19 Control Measures | Dengue Control Measures |
|---|---|---|
| Diagnostic Tests | PCR from respiratory samples, rapid antigen tests | PCR and ELISA from blood/serum samples |
| Patient Isolation | Isolation wards with negative pressure rooms | Clinical observation and isolation to prevent hospital outbreaks (not person-to-person) |
| PPE Requirements | Masks (N95), gowns, gloves, face shields | Gloves, masks, and standard precautions |
| Air Management | 12+ air exchanges per hour, no air recirculation | Focus on preventing mosquito exposure in hospital |
| Staff Training | PPE protocols, donning/doffing techniques | Awareness of dengue clinical warning signs and infection control |
| Waste Management | Infectious waste segregation and disposal | Proper handling of blood-contaminated materials |
| Clinical Monitoring | Respiratory support, oxygen therapy | Fluid management, early detection of severe dengue |
| Community Measures | Social distancing, vaccination campaigns | Vector control, source reduction, community education |
Latest Updates
- Hospitals continue to enhance rapid diagnostic capabilities combining molecular and serological testing to manage overlapping epidemics efficiently.
- Technological integration such as paperless test requests and result sharing via digital platforms has minimized contact and improved sample tracking.
- Increased emphasis on multi-sector collaboration involving public health, environmental services, and clinical teams for better outbreak containment.
- Development of standard operating procedures for managing co-epidemics like COVID-19 and dengue, especially in tropical and subtropical regions.
- Implementation of innovative training programs using virtual reality and simulation to improve HCW readiness for infectious disease scenarios.
- Rising adoption of telemedicine and remote patient monitoring to reduce hospital visits and prevent on-site transmission.
Hospitals globally are adapting continuously to the evolving challenges posed by infectious diseases, focusing on strengthening IPC practices, infrastructure, and workforce capability to provide safe and effective care.